Basal Body Temperature (BBT)
Basal Body Temperature (“BBT”) Tracking
By Cassandra
Why would you track your basal body temperature?
Your basal body temperature is your body temperature taken immediately upon waking. This temperature, when taken daily and plotted on a chart, can help identify the status of your fertility at various times throughout your monthly cycle. Women often use BBT tracking to assist them in becoming pregnant. It may also help determine inconsistencies in a woman’s cycle which may be affecting her ability to conceive. Finally, women also use BBT tracking to aid in their efforts to avoid pregnancy.
What you can expect
BBT Tracking is relatively simple and inexpensive. You will need a thermometer that shows temperature with at least one decimal, paper, and a pencil. Digital thermometers are often the most accurate and reliable but you may use a glass thermometer if you wish, so long as it is a “basal body” thermometer. Ear thermometers are not recommended as they are often not as reliable.
You may begin charting at any time in your cycle so long as you are sure to record the temperature on the correct cycle day area of the chart you are using. Cycle Day One is always the first day of your period.
Each morning upon waking, prior to any activity, take your temperature and note the result on a sheet of paper. It is preferable to take your temperature even before speaking as your temperature will be higher if you move around first. This will skew your charting results. In addition, you should try to take your temperature at approximately the same time each day and always after at least 5 hours of sleep (3 hours uninterrupted sleep minimum). Your temperature rises approximately .2 degrees per hour throughout the morning (or will be approximately .2 less for each hour earlier). This change in temperature (due to inconsistent timing) will skew your charting results.
When writing down your daily temperature, it is helpful if you also note any other symptoms you may have such as breast tenderness, headache, moodiness, consistency of cervical mucous, and cervical position. You can note anything that seems to be a part of your monthly cycle. Although technically not required to use BBT tracking, these additional notes will help you read your charts with more accuracy.
It is easiest to see the patterns in each cycle’s temperatures if you chart them on a graph. Most women use a chart something like the sample below. The following websites offer printable, downloadable or online charts:
http://www.fertilityfriend.com
http://www.tcoyf.com
http://conception.parenthood.com/bbt_chart.html
There are many more websites out there that offer similar charts. You can find them by searching the web for “basal body temperature” or “basal body chart”.
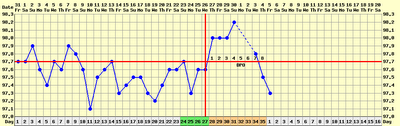
Sample BBT Chart
After you have charted your temperature for a month or s,o you will probably begin to see a pattern arise. What you will be looking for is a temperature increase of at least 0.4 degrees over a 48 hour period. This shift usually coincides with ovulation and marks the end of the follicular phase of your cycle.
Usually, the temperature will then drop and rise again during the luteal phase of that cycle (as shown in the sample chart). Most often the temperature will drop around the time of onset of menses. If your temperature remains high during the latter portion of your cycle for 18 days or more, you should test for pregnancy.
You may be able to see the shifts between cycle phases easily on your chart. However many women also draw a “coverline” on their chart to help them identify the cycle shifts. This is done by looking at the highest temps taken during the end of your period and looking for the first day your temperature rises at least 0.2 of a degree higher than the end of period high temps. The cover line is drawn one-tenth of a degree above the highest of the high days preceding the rise. (See sample chart).
Note that recording of additional symptoms such as cervical mucous and position add additional clues as to the status of your facility at any given time during your cycle. This article does not address those items but you may want to check the websites above for more information on this.
Problems that may arise and ways to troubleshoot
The birth control pill, coming off of the birth control pill, and recent miscarriage or childbirth may affect your chart and make it appear irregular or inconsistent.
Illness and/or fever may also skew your results. Unusual events such as travel, alcohol consumption, a restless night or extreme stress may also have an effect on your results. If you have a temperature on your chart which you think may be artificially high or low because of these circumstances or due to taking your temperature at a time outside of the norm for you, it is sometimes helpful to highlight or circle those temperatures on the chart so that you remember not to look as closely at them as you interpret your chart.
If you experience extremely erratic or unusual temperatures be sure to double check that you are taking your temperature at the same time each day and prior to any activity. You may want to note the time you took your temperature on your chart each day to help with this.
If you wake up an hour or two before you usually take your temperature and just have to go to the bathroom or something, it is better to take your temperature at that time rather than getting up, and then going back to bed until it is time to take your temperature. Getting up and going back to bed for an hour or two will interrupt you sleep/temperature pattern (remember – your temperature should be taken after at least five hours of uninterrupted sleep).
If you notice that you are not finding the ovulation spike in your temperatures or that your charts are not making sense to you, it may be helpful to take them to your OB/GYN and seek his or her input.
Personal Tips
Until you get used to taking your temperature regularly, it may be difficult to remember every morning. I place the thermometer right on top of my alarm clock when I go to bed so that I can’t even hit “snooze” without grabbing the thermometer.
A great resource for learning to chart your basal body temperature is the book Taking Charge of Your Fertility by Toni Weschler, MPH.
I have found that BBT charting is great for getting a handle on approximately when you ovulate each month but is more of a look backward. So basically, you don’t know you’ve ovulated until you’ve already charted it and passed it. I often use the charting in combination with ovulation predictor kits when trying to get pregnant.
If you are seeing an OB/GYN for help with a fertility issue you may want to take your charts to your next appointment. My OB was able to use my charts to help determine how to treat me.
July 26, 2006 5 Comments
Diagnosis: Male Factor
Diagnosis: Male Factor
by Bea
What Male Factor Infertility Means and Its Impact on Fertility
Male factor infertility (MFI) means, simply put, that a man has a lower than normal chance of fertilising an egg without assistance. “Lower than normal” may mean anything from slightly reduced to zero chance.
MFI is common. Statistics show 30-40% of infertile couples suffer exclusively from male factor infertility, 30-40% exclusively from female factor infertility, and the rest from unexplained or combination factors involving both partners. This serves to highlight the fact that infertility is far from being a female-only problem–in fact, the problem is equally likely to rest with the male. The reason behind a man’s infertility is mostly elusive and unlikely to change the options for treatment.
Happily, MFI carries a generally good prognosis as long as some sperm are being produced. Amongst IVF patients, only those with tubal infertility are more likely to conceive. On the downside, if MFI is severe enough there is no hope of a “surprise pregnancy”.
Sperm may lack the ability to fertilise an egg for one of a number of reasons:
- Count: Contrary to what you were told at school, it actually takes a minimum of between half and one million healthy, rapidly-motile sperm to fertilise a single egg. This equates roughly to a post-wash count of five to seven million sperm per ml. This is because sperm work together to navigate their way through the inhospitable environment of the female reproductive tract. It’s physcially impossible for a single sperm to make a successful journey all by itself. So much for “it only takes one”. Count may be reduced because of lack of production in the testicles, or failure of sperm to get from the testicles into the ejaculate (for example blockage/previous vasectomy).
- Motility: Only rapidly motile sperm can reach and penetrate an egg. Even if fertilisation happens in vitro, motility is required to get through the “shell” of the egg.
- Morphology: This is much less important than you might think, especially if you are using ICSI. The DNA contained in the head of abnormally-shaped sperm is just fine.
- Anti-sperm Antibodies: Antibodies can cause a loss of motility, the clumping together of sperm, and the inability for the sperm to fertilise an egg. This is much more common in men who have had vasectomies.
- Sperm DNA Fragility: This means the DNA carried in the head of the sperm is damaged. The somewhat controversial belief is that higher levels of DNA damage will lead to greater numbers of genetically abnormal embryos being formed, resulting in implantation failure and early pregnancy loss.
Diagnostic Process
Standard Semen Analysis: This will give an indication of count, motility and morphology. It will also give details of any other cells – for example white blood cells – which may indicate infection.
Post-wash Semen Analysis: Some specialists like to analyse the sample after washing, as if for an IUI. This will give a more accurate indication of whether the sample is good enough for IUI or whether IVF will be needed.
Antibody Tests: This is most reliably done on a semen sample. Tests include the immunobead assay and the mixed agglutination reaction. Results are given as a % of sperm with antibodies attached.
Sperm Chromatin Structure Assay: This is the test for DNA fragility. It’s performed on a semen sample. Results are given as a DNA Fragmentation Index which aims to indicate what % of the DNA is damaged.
TESA/MESA/testicular biopsy: If no sperm at all are found in the ejaculate, an aspirate or biopsy may be taken to hunt for sperm in the epididymus or testicle. There’s a big difference between a few sperm and no sperm at all.
Hormone assays: This is a blood test. FSH means much the same thing in men and women. High FSH indicates poor response by the testicles (or ovaries). Testosterone is usually also measured, and sometimes other hormones such as LH and prolactin.
Karyotyping: Some males have abnormal genes which affect fertility, such as the XXY karyotype which is known as Klinefelter’s Syndrome, or the cystic fibrosis gene which can cause anatomical defects in the sperm transport system. Balanced translocations can also occur in males as well as females.
Physical examination and ultrasounds: You may be referred to a urologist for physical examination and ultrasound of the testicles and prostate. Two of the most common things to look for are varicocoeles and prostatic disease.
Treatment Options
Treatment of MFI is centred on IUI, IVF, and ICSI. IUI can be used to give a marginally poor ejaculate a “head start”. IVF is used for more severe male inferility, and ICSI is used where the severity is such that sperm are no longer able to penetrate the egg by themselves at all. TESA/MESA or testicular biopsy are sometimes used to retrieve sperm, especially if none are present in the ejaculate. Some couples use donor sperm with IUI or IVF.
Many other options have been suggested. It’s important to note that because it takes a while for sperm to be produced, any treatment which aims to improve semen quality will take three to six months to produce results.
Lifestyle factors such as overheated testicles (sauna/hot baths), smoking, or drug use can affect semen quality. These must be eliminated. In a few cases, this might be enough to resolve the problem.
Many dietary supplements, naturopathic remedies, and alternative therapies have been suggested over the years, including arginine, B vitamins, coenzyme Q10, SAMe, ginseng, vitamin C, zinc, L-carnitine, co-enzyme Q10, vitamin E and selenium, omega 3 fatty acid supplementation, and acupuncture. Sadly, studies fail to consistently support any benefit. However, when used as recommended there seems to be no harm, either.
Hormonal supplements are used by some specialists. Supplementing directly with testosterone seems to actually reduce male fertility, but clomid and FSH have been used to stimulate testicles into production. A limited number of studies show a marginal benefit, but not enough to replace the use of IVF/ICSI.
Sperm DNA fragility is treated using ICSI, which seems to produce a higher pregnancy rate than plain IVF in this group, and also TESA/MESA, the aim of which is to use the freshest sperm possible, based on the theory that most DNA damage happens whilst the sperm is being stored in the body. Men may also be advised to ejaculate frequently (ie daily) to reduce storage time.
IVF is the most successful treatment for antisperm antibodies, with ICSI used if fertilisation fails to occur. IUI is also an option in some cases.
Variocoelectomy remains controversial. Some studies show benefits and others show no benefit at all. Some specialists believe there are select groups of patients in which the surgery is worthwhile. Be sure to discuss the pros and cons fully with your doctor.
Vasectomy reversal is most successful in cases where modern techniques have been used, and where the vasectomy was fairly recent (less than a couple of years). A succes
sful reversal produces sperm in the ejaculate but count, motility and antibodies may still warrant assisted conception. Discuss the pros, cons, costs and chances of success carefully with your doctor prior to surgery.
Infections, prostatic disease or other conditions should be treated as indicated. If there has been prolonged or severe insult to the testicles, assistance may still be needed to achieve pregnancy.
Personal Experience
It’s pretty clear from our semen analysis that IVF/ICSI is the only way we’re going to be able to achieve a pregnancy using our own gametes. Obviously this is not good news, but at least we have the chance to try. Our other options are sperm/embryo donation or adoption. No good reason has been found for our diagnosis, but the chicken pox Mr Bea contracted for the first time at sixteen years old is a possible culprit.
The biggest thing that strikes me about male factor infertility is the stigma. There are few men who are confident enough to talk about their diagnosis openly, and I find myself restricted from talking about our problems with friends and family at the express request of my husband, who wants his diagnosis to remain private. If I do tell someone we’re doing IVF, it’s automatically assumed we have a female factor problem.
July 26, 2006 13 Comments
International Adoption: Guatemala
International Adoption: Guatemala
by Erin
Note that the continuation of adoptions of Guatemalan children to US citizens is in jeopardy due to the US ratification of the Hague Convention in 2007. More information can be found at guatadopt.com.
Advantages to the Guatemala Program
- Foster care: Most adoptable children in Guatemala are in foster homes living in a family environment, not orphanages in which they may have very little one-on-one time with their caregivers. We know that a person’s early months are crucial to later development; the more physical, mental, and emotional stimulation an infant gets, the better.
- Information about the birth family: For relinquishment cases, which make up the majority of adoptions in Guatemala, a social worker interviews the birth mother to learn about the circumstances of the relinquishment and make sure she understands the decision to terminate her parental rights. Information about the birth family (in addition to a photograph of the birth mother and child taken at the time of the DNA test) is given to the adoptive family, who can then share this information with their child.
- Possibility of meeting the birth mother: It is uncommon in international adoption for adoptive parents to have the opportunity to meet the child’s birth mother. In relinquishment cases in Guatemala, however, it is possible if the birth mother agrees to it and your agency/attorney allows it.
- Infant referrals: Newborns are available for referral in Guatemala, and by the time the process is complete, the children are generally between 5-8 months old.
- Healthy children: Most children are relinquished due to circumstances of poverty, not because of they have physical or mental disabilities. Disorders such as Fetal Alcohol Syndrome are not prevalent in Guatemala.
- Frequent updates: Many agencies provide adoptive parents with monthly medical updates and photos. Adoptive parents find joy in the new photographs and comfort knowing that the child is receiving regular medical care.
- Relatively predictable timelines: Although timelines certainly fluctuate, adoptive parents do have a rough idea of how long each step in the process takes.
- Short in-country stay: Whereas some countries require at least one adoptive parent to stay up to a few months in the country, in Guatemala the stay is only a few days (adoptive parents can also choose to have an escort bring the child to the US in their stead). This means fewer food and lodging expenses for adoptive parents; if you are taking a leave from work, it also allows more time with the child once you are back home in the U.S.
- Ability to visit: For adoptive parents who are eager to visit the country of their child’s birth and begin the bonding process early, the ability to visit their child during the adoption process is a wonderful opportunity. Adoptive parents are encouraged to visit the baby in Guatemala before taking custody, so you can bond with the child very early in his or her life. In fact, if they wish, they can stay in Guatemala for 6-8 months and foster their own child.
- Geographical proximity: Being in Central America, Guatemala is closer than most other countries that allow international adoption to the U.S. This proximity makes it more viable for adoptive families to travel back to Guatemala as the child grows older.
The Process
The Guatadopt.com Resource Center provides very detailed information about the steps in the Guatemalan adoption process.
Resources
Guatadopt.com: Provides news, message boards, and information about the Guatemalan adoption process.
Soul of Adoption Guatemala forum
GuatemalaAdopt listserver, otherwise known as “The Big List”. Directions to subscribe can be found on guatadopt.com.
July 26, 2006 2 Comments
Choosing a Sperm Donor
Choosing a Sperm Donor
By DI Mom
Why Would You Be Using a Sperm Donor?
Those most likely to use a sperm donor are heterosexual couples with male-factor infertility, lesbian couples, and single mothers by choice (SMBC).
[Remember that many people fall into the male-factor category including those who knew prior to trying-to-conceive that they would have trouble producing sperm including those who have a prior history of cancer, spinal cord injury, or a genetic illness. Some people who can produce sperm but are carriers of a genetic illness may choose to use donor sperm in order to not pass along those genes–Mel]
What to Expect?
The first step is usually to meet with a reproductive endocrinologist (RE). Your RE will perform various blood tests and ultrasounds on you, and your partner if necessary, to confirm the cause of the infertility, to rule out any STDs, and to verify that your cycle and hormone levels are with a normal range. You may also be required to undergo a psychological assessment.
You then need to select the sperm donor that you would like to use. The first decision is do you want a known donor that is chosen by you or do you want to use a donor from a cryobank?
Some women feel very strongly that the donor have a genetic tie to her partner. In this case, the couple may approach a male relative and ask him to be a donor. The other option is to ask a family friend to be a donor. If this is the path that you choose, you should consider what tests should be performed to verify your donor’s health, how utilizing a known donor may affect future family dynamics, and other unique challenges that may arise. Your RE can suggest various tests and resources if you prefer this route.
If you decide that you would prefer to use a more anonymous cryobank (AKA sperm bank), there are various levels of service that you should consider before you choose your bank. For example, some banks participate in an “open donor” program in which information about your donor may be released when your child turns 18. Others do not require that you be under a physician’s care, if you decide that you would prefer to perform the insemination at home. Many have online support groups for their clients. Some provide photos of the donors as children or audio of interviews with the donor. Once you determine which cryobank you would like to use, it is time to choose your donor.
All of the larger cryobanks have their donor list available in a searchable online document. Before you begin, it is helpful if you choose which characteristics and traits are important to you. If you are unsure if you will disclose to your child about your use of donor insemination (DI), you may wish to choose based on your partner (i.e. height, weight, eye color, hair color and type, blood type, etc.). Also, you can eliminate donors with a genetic history that you feel is problematic such as cancer or alcoholism. Many banks will perform photo matching where you submit a photo of your partner and they will suggest donors who have similar features.
You will also need to choose the specimen type, Intracervical Insemination (ICI) or Intrauterine Insemination (IUI). Discuss with your RE the pros and cons of the two types.
Once you have selected your donor, the next step is usually to contact the cryobank and place your order. You may have to pre-register with the cryobank so allow yourself enough time for the paperwork to be processed. Your order will then be delivered in a special nitrogen tank (dewar) and your doctor will help you determine your insemination date and time based on your ovulation cycle.
Problems that May Arise and Ways to Troubleshoot
The donor that you choose may be very popular, especially if he has reported pregnancies, so it is a good idea to have several alternatives in mind in case your top pick is not available. Also, cryobanks will keep specimens in quarantine for several months while some of the tests are run so a donor that is not available for your current cycle may be available for subsequent cycles. You can always ask the cryobank how many specimens are in quarantine and when is the expected release date.
Chart your ovulation date for several months prior to your insemination cycle so that your order will arrive at the appropriate time.
Personal Tips
Read over the personal tips that are in the Choosing a Donor Egg write-up. Most also apply to using donor sperm.
Before you begin, check with your insurance provider regarding what fertility tests and treatments they will cover. Get everything in writing and know the appeals process in the event your claim is denied.
Think ahead. If you think that you may want more than one child and it is important to you that they be genetically related, choose a donor with plenty of specimens available. When you become pregnant, you may purchase additional specimens and have them stored at the cryobank until you need them. If the specimens never leave the cryobank, you may be able to be refunded some of your money if you later decide that you no longer need them but check with your bank as to their specifics.
Depending on which bank you use, the type of specimen (ICI or IUI), whether you are under a doctor’s care or are performing the insemination at home, and other factors, one DI cycle will likely cost $1000-$5000. Before you begin, you should honestly assess your financial situation and determine how many cycles you can afford. Success rates are difficult to determine but are usually quoted as being around 10%. Some will become pregnant on the first try and others will require 12 cycles or more. You will need to decide what is right for you.
If you would like to read more about the in-and-outs of donor insemination, I highly recommend Helping the Stork: The Choices and Challenges of Donor Insemination by Carol Vercollone, Heidi Moss, and Robert Moss (Wiley, 1997).
July 26, 2006 2 Comments
Diagnosis: Anovulation
Diagnosis: Anovulation
by Amy
What Anovulation Means and Its Impact on Fertility
Anovulation is the word used to describe a woman who does not properly develop and release a mature egg every month (ovulate). Women who are consistently anovulatory often have long, irregular cycles, sometimes not having a period for months or even years. The most common cause of consistent anovulation is Polycystic Ovarian Syndrome (PCOS). Other possible causes of anovulation include high stress, excessive physical exercise, obesity, overeating, birth control, hormone imbalances (thyroid, testosterone, prolactin, etc…), breast feeding, and even Premature Ovarian Failure (POF). Anovulation can be continual (such as with PCOS or other hormone imbalances) or it can be temporary (such as with stress or breast feeding). Doctors agree that even normally ovulating women can experience one or two anovulatory cycles per year. Anovulatory cycles obviously cannot result in a pregnancy (no egg = no baby). Medical intervention is needed when women are consistently anovulatory.
Diagnostic Process
Anovulation is diagnosed either via ultrasound and/or bloodwork (usually both). An ultrasound can reveal whether or not your ovaries are polyfollicular (PCOS). Bloodwork can be used to test hormone levels such as thyroid, prolactin, progesterone, and FSH levels (which can indicate POF).
Treatment Options
Treatment will depend on your diagnosis. If you are diagnosed with PCOS, you’ll probably start with clomiphene citrate (Clomid) and/or metformin (Glucophage). Generally, PCOS is treated with a combination of both. Specific medications and/or dosages will be adjusted accordingly, depending on each women’s individual response. For women who are anovulatory due to stress or exercise or if anovulation is deemed temporary, simple lifestyle changes can cause ovulation to return. For women with POF, treatment will probably be more in-depth and often includes In-Vitro Fertilization, sometimes requiring donor eggs.
Personal Experience
I, myself, am consistently anovulatory. However, my situation is slightly different because my anovulation is unexplained. All my hormone levels have been repeatedly checked and everything is within normal ranges. I do not have PCOS or POF. I am not stressed or obese, and I can safely say that I do not excessively exercise. No one has been able to tell me why I don’t ovulate. I did ovulate once on Cycle Day 50 of an unmedicated cycle and became pregnant (that pregnancy ended in miscarriage). Thankfully, under the care of a knowledgable Reproductive Endocrinologist (RE), we learned that with the right dose, I respond beautifully to Clomid. I have done nine Clomid cycles, eight of them ovulatory (my first round of 50mg of Clomid was anovulatory). I became pregnant on three of the eight ovulatory cycles. Unfortunately, all ended in miscarriage due to chromosomal issues having nothing to do with the Clomid. I am still using the Clomid (as of this writing, I am in the middle of my ninth Clomid cycle) to induce ovulation.
July 26, 2006 23 Comments